Health Outcomes and Policy
In large national registries and datasets, we have defined both methodologic best practices for rigorous investigation and identified adherence to evidenced-based cardiovascular care
Methodological Best Practices
Clinician Trends in Prescribing Direct Oral Anticoagulants for US Medicare Beneficiaries
Transition to the ICD-10 in the United States
An Emerging Data Chasm
Adherence to Methodological Standards in Research Using the National Inpatient Sample
Administrative Codes for Capturing In-Hospital Cardiac Arrest
Acute Cardiovascular Care
We have evaluated national patterns of care and outcomes of patients hospitalized with cardiovascular conditions, and the concordance of care practices with clinical guidelines
Revascularization Practices and Outcomes in Patients With Multivessel Coronary Artery Disease Who Presented With Acute Myocardial Infarction and Cardiogenic Shock in the US, 2009-2018
Temporal Trends in Heart Failure Incidence Among Medicare Beneficiaries Across Risk Factor Strata, 2011 to 2016
Role of Hospital Volumes in Identifying Low-Performing and High-Performing Aortic and Mitral Valve Surgical Centers in the United States
Trends in the Use of Percutaneous Ventricular Assist Devices:
Analysis of National Inpatient Sample Data, 2007 Through 2012
Cardiac Arrest
We have defined a series of quality measures for the care of patients with in-hospital and out-of-hospital cardiac arrest
Time in therapeutic range for targeted temperature management and outcomes following out-of-hospital cardiac arrest
Pulselessness After Initiation of Cardiopulmonary Resuscitation for Bradycardia in Hospitalized Children.
Association Between Hospital Recognition for Resuscitation Guideline Adherence and Rates of Survival for In-Hospital Cardiac Arrest
Hospital Variation in the Utilization and Implementation of Targeted Temperature Management in Out-of-Hospital Cardiac Arrest
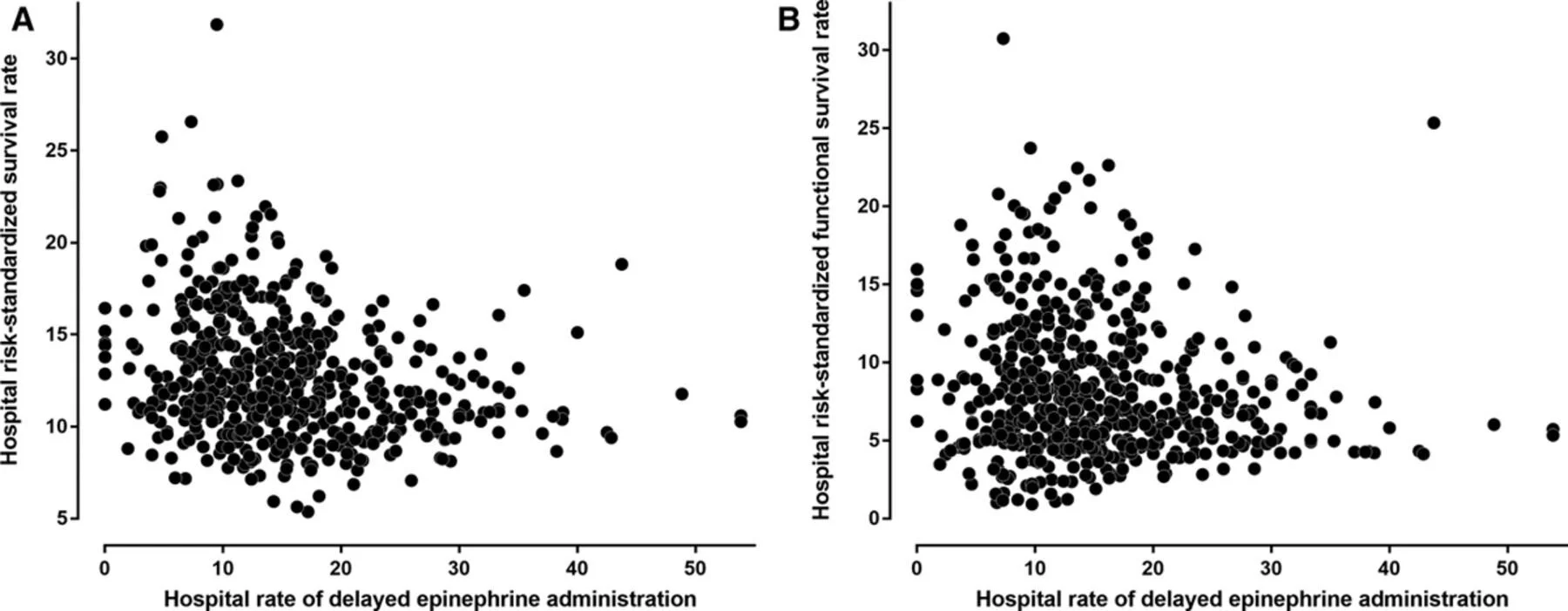
Hospital Variation in Time to Epinephrine for Nonshockable In-Hospital Cardiac Arrest
Our work focuses on a rigorous evaluation of health policies and their association with cardiovascular health and outcomes
Financial Toxicity from Cardiovascular Care
We have uncovered a large burden of financial toxicity from healthcare among patients with cardiovascular disease, a function of both their emergency and acute care needs as well as out-of-pocket expenses on health insurance and health maintenance
Out‐of‐Pocket Annual Health Expenditures and Financial Toxicity From Healthcare Costs in Patients With Heart Failure in the United States
Financial Toxicity in Atherosclerotic Cardiovascular Disease in the United States: Current State and Future Directions
Cost-Related Medication Nonadherence in Adults With Atherosclerotic Cardiovascular Disease in the United States, 2013 to 2017.
Association of Out-of-Pocket Annual Health Expenditures With Financial Hardship in Low-Income Adults With Atherosclerotic Cardiovascular Disease in the United States
Burden of Catastrophic Health Expenditures for Acute Myocardial Infarction and Stroke Among Uninsured in the United States
Hospital Readmissions
In a series of investigations, we rigorously evaluated the effects of the Hospital Readmission Reduction Program on readmissions, mortality, and post-acute care.
Post-discharge acute care and outcomes following readmission reduction initiatives: national retrospective cohort study of Medicare beneficiaries in the United States
Evaluation of 30-Day Hospital Readmission and Mortality Rates Using Regression-Discontinuity Framework
Association of the Hospital Readmissions Reduction Program With Mortality During and After Hospitalization for Acute Myocardial Infarction, Heart Failure, and Pneumonia
Burden of Catastrophic Health Expenditures for Acute Myocardial Infarction and Stroke Among Uninsured in the United States
Therapeutic evaluation
We have evaluated both the effectiveness and risk-stratification tools used to define the need for therapy in different populations